Policy Brief: Staci Rising Paquet
Study Authors: Katie Bailey, Program Analyst, IU Public Policy Institute, and Brad Ray, Director of the Center for Criminal Justice Research
The City of Indianapolis has made strides in addressing the high rates of involvement of people with mental health and drug issues in the criminal justice system, a phenomenon spanning the country. A pilot program in the IMPD East District uniquely combines police, paramedics and behavioral health specialists to act as first-responders to any emergency calls related to mental health or substance use in the district. Researchers from the Center for Criminal Justice Research at the Indiana University Public Policy Institute (PPI) collected and analyzed data on the first five months of this program’s pilot operation.
“While initial findings show positive feedback for the MCAT pilot program, more research is needed to fully understand the effectiveness of the program,” says Tom Guevara, director of the Indiana University Public Policy Institute. “There’s no question that leading-edge programs like MCAT can have a tremendously positive impact on our city as a whole. We found, however, that a lack of outpatient treatment options and other barriers to expanding the program must be addressed in order to maximize the impact of the MCAT helping to address serious mental illness and substance abuse problems for Indianapolis.”
According to the Marion County Sheriff’s Office, approximately 40% of detainees in the county’s jails at any one time suffer from mental illness, resulting in $8 million of medical care and services annually. In addition, roughly 85% of detainees with a mental illness are also diagnosed as suffering from substance abuse issues. In May 2016, Indianapolis Mayor Joe Hogsett formed the Criminal Justice Reform Task Force to address, among other issues, the significant number of individuals entering the criminal justice system with mental health or substance abuse issues. This resulted in the establishment of a Mobile Crisis Assistance Team (MCAT) pilot program that integrated Indianapolis Metropolitan Police Department (IMPD) officers, Indianapolis Emergency Medical Services (IEMS) paramedics, and mental health clinicians from Eskenazi Health Midtown Community Mental Health (Midtown) into teams to respond to emergency calls involving people with behavioral health and/or substance use issues.
The pilot program aimed to divert those people to behavioral health providers and social services instead of the criminal justice system, and to relieve other first-responders from the scene of these time-consuming and complicated emergency situations. Dozens of similar teams currently operate in North America and have several common goals. As a relatively new idea, only a handful of studies have examined the effectiveness of these teams. However, existing studies have found that co-response teams are cost effective, well-received by the communities they serve, and reduce burdens on the criminal justice and healthcare systems. The Indianapolis MCAT pilot project launched on August 1, 2017. Four MCAT units were formed for 24/7 availability within the boundaries of the IMPD East District. MCAT serves as a first-response unit, responding to a crisis scene via self-dispatch or at the request of other first responders.
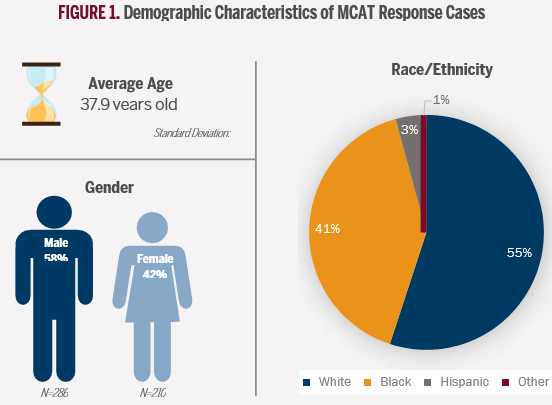
The Center for Criminal Justice Research at the Indiana University Public Policy Institute evaluated the pilot program using data from MCAT run reports between August 1, 2017 and December 9, 2017. Additionally, key stakeholders and program designers were interviewed, focus groups were held with MCAT team members, and ride-alongs were completed.
FINDINGS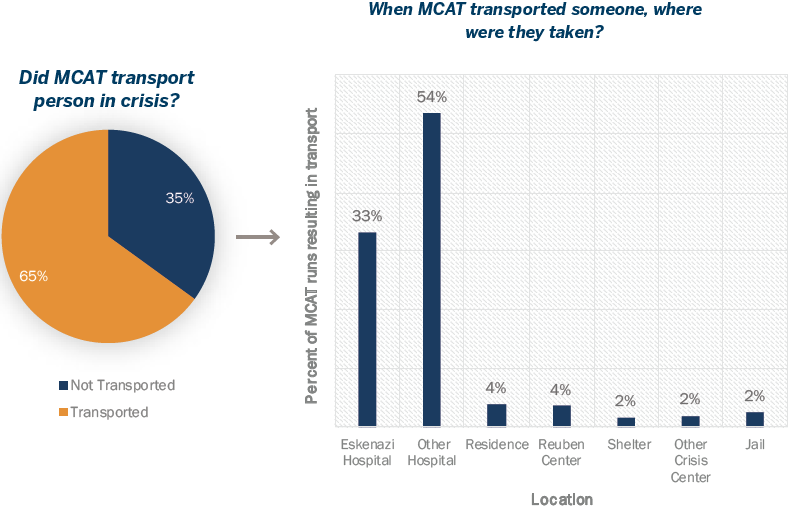
• 59% of MCAT responses involved mental health crises, followed by overdose or substance abuse (35%) and suicide attempts or self-harm (34%)
• The MCAT has broad support among surveyed police officers in the IMPD East District, several of whom requested greater MCAT availability
• In 2/3 of runs, MCAT units were able to relieve other first response units from the scene of an emergency, allowing them to return to service
• MCAT is much more likely to transport a person to receive medical treatment than to arrest; a person was transported to jail in less than 2% of all responses during the pilot
• MCAT units encountered a small subset of “frequent flyers”—individuals receiving multiple MCAT responses during the study period—and doubled efforts aimed at reducing their use
of emergency resources through treatment connection
• A lack of long-term treatment options for people with mental health and drug-related emergencies limits MCAT’s impact
• An initial absence of detailed policies and procedures allowed for real-time learning, but led to confusion amongst MCAT team members regarding what they should or should not be doing and resulted in inconsistencies amongst teams
• Triangulation of collaborating agency information on persons experiencing emergencies allowed MCAT to better prepare crisis responses and facilitated re-engagement with treatment for MCAT patients
• Support and buy-in from city officials in addition to a history of collaboration with mental health specialists facilitated the coordination of this innovative initiative across three agencies
• Team building exercises during MCAT training emerged as a salient facilitator to implementation of the MCAT pilot program
• There is still a need to coordinate and clarify MCAT goals and responsibilities with external actors such as other first responders, community mental health initiatives and treatment providers
CONCLUSION & RECOMMENDATIONS
There are several policy implications from this pilot study. First, the creation of a program coordinator position for the MCAT units can provide oversight and ensure consistency among units, be a liaison between leadership and MCAT teams, and enhance communication and relations with external stakeholders. Second, community treatment resources must be expanded in the Indianapolis area, as lack of local treatment options was cited as a barrier by both MCAT stakeholders and participants of previous studies of similar teams across North America. Third, consideration should be given to partnering with other Indianapolis treatment providers to expand information sharing among MCAT teams and providers beyond Midtown. This study represents a brief snapshot of the first five months of the MCAT program, but additional research is needed to examine MCAT’s effectiveness. First, data from MCAT responses needs to be linked to other available information such as jail and IEMS data to better understand the program’s effects on patients’ public safety outcomes. Second, the MCAT runs need to be compared to similar calls for service where MCAT was not available to respond to understand the differences in how these crises are handled. Finally, researchers need to better understand the perceptions and experiences of individuals who are consumers of MCAT services through one-on-one interviews and linkage to information related to individuals’ treatment engagement.
 port here
port here